What is the cornea?
The cornea is the front surface of your eye which light passes through in order for you to see. It is the transparent elliptical surface of your eye that allows for good vision. Good vision is only achievable if your cornea is clear and healthy. Any damage to this structure such as scarring or swelling causes your vision to be blurry. If all options have been exhausted to provide clear and comfortable vision, your eye doctor may recommend surgery to correct the problem. This may be necessary if vision can no longer be corrected with the use of glasses or contact lenses or if painful swelling cannot be resolved with medication. Corneal transplantsinvolve replacing your current diseased cornea with a clear, smooth, and healthy cornea. This new cornea comes from human donors. Rest assured, all donor corneas are put through extensive testing to make sure they are safe and healthy to use.

What are the benefits of corneal transplant?
A corneal transplant can help restore the eye to it’s former condition. This allows for sight restoration in conditions like keratoconus where the shape of the cornea prevents crisp clear vision. It allows for pain reduction in conditions where the cornea is diseased and painful. It allows for an improvement in appearance for patients with cloudy or opaque corneas.
Who gets corneal transplants?
Corneal transplants are done for patients with a severely damaged cornea (front of eye). This can involve swelling, distortion, and painful corneas. A corneal transplant may be performed for patients who experience these conditions in order to improve their quality of life through improved vision and cosmesis while simultaneously reducing pain.
Some examples of conditions that may require a corneal transplant are:
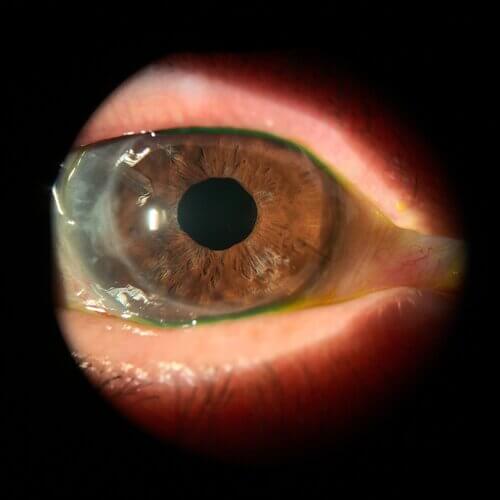
Keratoconus
- Fuch's dystrophy
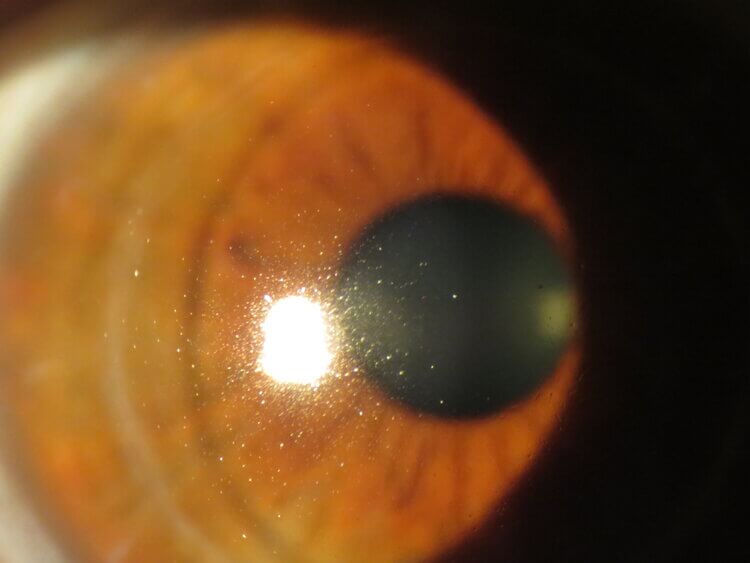
- Corneal scarring
- Clouding corneas
- Swollen corneas
- Corneal ulcer
- Patients with eye surgery complications
- Thin corneas
What are the risks?
Like all surgeries, corneal transplants come with their share of risks. However, the procedure is relatively safe and carries a small risk of complications. Some examples of known associations are:
- Eye infection
- Swollen corneas
- Cataracts or clouding of the eye’s lens
- Issues with the stitches placed on the donor tissue
- Rejection of donor tissue
See your eye doctor right away if you feel you are experiencing any new symptoms.
What are the signs of a corneal transplant rejection?
Corneal transplants involve bodily tissues that are from a donor. In some cases, the body may interpret this new tissue as infectious and the body’s immune system will attack the new cornea. This is considered a corneal transplant rejection and typically requires medical treatment. Some symptoms associated with corneal transplant rejection include:
- Blurry vision or loss of vision
- Redness
- Light sensitivity
- Painful eyes
If detected early enough, the majority of rejection cases can be reversed. Rejection can happen in the early stages post surgery or can happen even several years after surgery. However, the benefits of treatment often outweight the small risk of rejection. Your eye doctor can go over your benefits and risks of procedure with you to determine if this procedure is right for you.
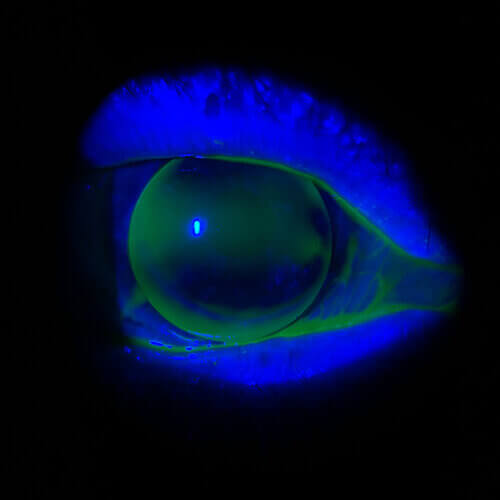
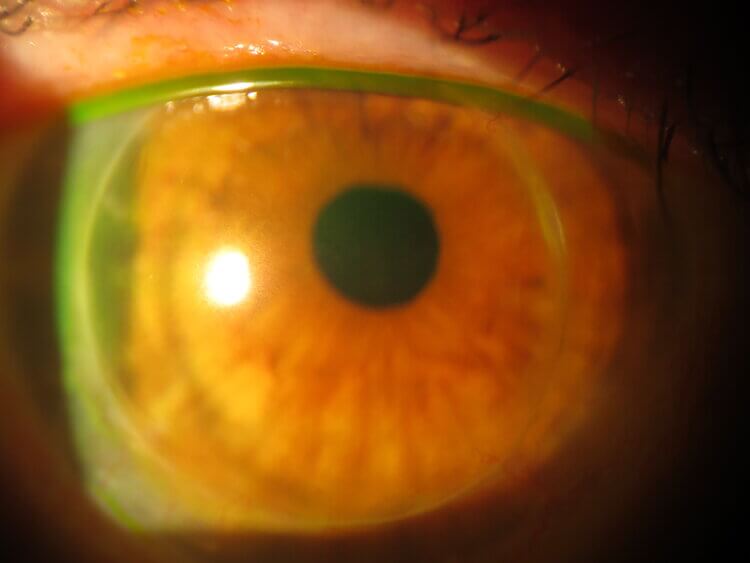
What to expect and how to prepare for surgery
Prior to a corneal transplant surgery, your eye doctor will assess the health of your eye during a comprehensive eye exam. Measurements will be taken to determine the size of donor cornea you will need and determine any potential risks you may have following surgery. Active eye infections or eye conditions must be resolved prior to surgery to minimize your risk of complications. Any active conditions decrease your chances of surgical success and increase the likelihood of graft rejection. Go over your current list of medications and supplements to ensure they are safe to take prior to surgery. Your eye doctor may have you discontinue some drugs before your surgery. On the day of your surgery, the use of medications to help with numbing of the eye as well as sedatives to help you relax. You will not be put to sleep during the procedure but you will be comfortable and will not feel any pain. However, general anesthesia can be administered if preferred. The surgeon will cut through the cornea using a laser to remove a button sized piece of tissue like a cookie cutter. How deep the cut will be would be dependent on the type of corneal transplant you get. The most common procedure, termed penetrating keratoplasty, requires a full thickness removal. This means all layers of the cornea will be removed. Once the old tissue is out, the donor cornea is cut and fit into the opening. The new cornea is stitched into placed and will be removed at a later date. The entire procedure takes 1-2 hours.
How effective is a corneal transplant?
The results of the procedure depend on your state of vision before surgery as well as the reason for surgery. Most people who undergo corneal transplants experience at least a partial recovery of vision. Following surgery, you may notice your vision is temporarily worse than it was before surgery. This is because the eye is adapting to the new cornea. Give it a few months to experience the full benefit of treatment. This surgery doesn’t guarantee that you will not require corrective lenses such as glasses or contacts after. Due to the stitches placed in the eye, this may induce an uneven surface which can result in newfound astigmatism in your prescription. Your doctor can make adjustments to stitches to combat this as well as prescribe glasses or contacts to wear.
Post surgery expectations
Once your procedure is complete, you should expect to be on several medications and to wear an eye patch while your eye heals. The medications prescribed following surgery will be to help control swelling, pain, and reduce risk of infections. Your eye doctor will go over your necessary medications with you. Following the procedure, your cornea will be extremely delicate so you must take great care to protect your eye from injury. Expect some down time following the transplant and then slowly incorporate your daily activities back in. This includes exercise. Extra care must be taken indefinitely to avoid harm to the eye. Wear sunglasses to help protect the eye as much as possible. Follow ups with your eye doctor will be necessary to ensure no complications arise within the first year of surgery. See your eye doctor earlier than scheduled if you notice any changes in your vision or experience any trauma to the eye. Full visual benefits may take some time after surgery due to healing. Expect the recovery process to last up to 12 weeks.
Where does the donor cornea come from?
Like most organ donations, corneal transplants are done using deceased human donations. Corneal donations are not as hard to come by as other organs. Therefore, these are typically available as needed.
Can I become a corneal donor?
Anyone can become a corneal donor. The donors blood type does not need to match the recipients blood type. A corneal donor can restore vision in up to 2 people. If you are considering becoming a corneal donor then there are plenty of organizations available to help you sign up!
Procedure types
There are a few options when it comes to corneal transplants. Due to technological advances, there are a few procedures out there that require removal of different amounts of tissue. Speak to your eye doctor about which procedure is right for you. Some examples of available procedures are:
-
Full thickness corneal transplants
o A full thickness corneal transplant is referred to as a penetrating keratoplasty or PK. In this procedure, all layers of the cornea are removed and replaced with donor tissue. Due to the invasiveness of the procedure, it does involve a higher risk of rejection and a longer healing time.
-
Partial thickness corneal transplant
o Deep anterior lamellar keratoplasty or DALK involves replacing all layers except for the corneal endothelium. The endothelium is the innermost layer of the cornea. This provides a lower risk of rejection of the graft.
o Endothelial keratoplasty or EK involves the removal of only the innermost layer of the cornea. This layer is called the endothelium. This procedure leaves the rest of the overlying healthy corneal tissue in place and in tact. The surgeon will make a small incision in the cornea and place a thin disc of donor tissue in the back surface of the cornea. The use of air bubbles allows for positioning of the disc. No sutures are used. Some advantages of this over full thickness procedures involves faster recovery, less operating time, and minimal tissue removal. The minimal disruption of tissue reduces the patients risk of complications following surgery.